07 Mar Pulmonary Rehabilitation: Live Better and Live Longer
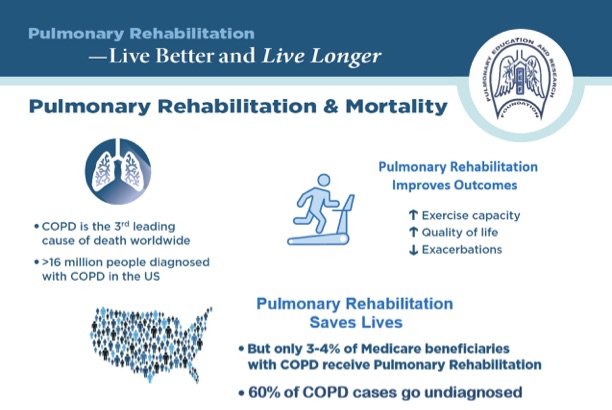
Over 16 million people in the US have COPD,1 and up to 60% go undiagnosed.2 COPD is the third leading cause of death globally.3 COPD and fibrotic lung disease, such as idiopathic pulmonary fibrosis (IPF), have no known cure and are associated with significant suffering and disabling symptoms.
Pulmonary Rehabilitation (PR) is the standard of care for persons with COPD and IPF, and it is associated with improved physical function, symptoms, mood, and quality of life. Although PR is well-established as a highly-effective treatment for COPD and other chronic respiratory diseases,4,5 in the US, only 3—4% of Medicare beneficiaries with COPD receive PR.6 Similarly low estimates exist for the rest of the world.7
Emerging data suggests a further benefit of PR: a reduction in mortality. A study by Lindenauer and colleagues found that in persons hospitalized due to exacerbation of COPD, pulmonary rehabilitation within three months of discharge vs. later or no PR was associated with a highly-significant lower risk of mortality at one year (hazard ratio, 0.63; i.e., a 37% lower risk of death over the year following discharge).8 The study utilized claims data of 197,376 Medicare beneficiaries discharged after hospitalization for COPD.
In persons with fibrotic interstitial lung disease (ILD), including IPF, Sabina Guler and colleagues demonstrated that those with greater improvement in exercise performance following PR (assessed by six-minute walk distance) had improved survival. Those persons with ILD who participated in at least 80% of planned PR sessions had a 33% lower risk of death.9 Both studies support PR as a high priority for persons with COPD and fibrotic ILD.
Patients suffering from COPD and fibrotic ILD should know that pulmonary rehabilitation not only has potential for helping them feel better and being more independent, but also living longer. We are asking for your support in communicating these important findings of improved survival after PR to providers and patients. Thank you in advance for your help and collaboration.
- Allergy & Asthma Network
 Alpha 1 Foundation
Alpha 1 Foundation- American Association of Cardiovascular Pulmonary Rehabilitation
- American Association for Respiratory Care
- American Academy of Allergy, Asthma & Immunology
- American Lung Association
- American Thoracic Society
- CHEST/American College of Chest Physician
- COPD Foundation
- Dorney-Koppel Foundation LAM Foundation
- Lung Transplant Foundation
- phaware Global
- Pulmonary Education and Research Foundation
- Pulmonary Fibrosis Foundation
- Respiratory Compromise Institute
- Respiratory Health Association
- Right2Breathe
- US COPD Coalition





Gilbert Brown
Posted at 17:34h, 20 MarchI am a 78 yr old male with COPD fev1 is 41 and was 52. I have had rehabilitation about 3 years ago and now I do it at home. I would like to know if what I am doing is good and I thought no pain no gain . I walk 15 to 30 minutes three times a week and Used to Walk 30 min three times a day I do weights 10 lbs up over head and curls at least 3 times a week and a arm machine for 5 min three times a day . Plus I cut grass and try to keep busy however I have to stop and rest and have over done it. Any help would appreciated .
Gil Brown
PERF
Posted at 14:22h, 25 MarchDear Gilbert,
You are amazing and I nominate you as poster patient of the month! The best way to keep helping yourself, Gilbert, is to help others. My suggestion is that you volunteer at your nearest Pulmonary Rehab program. You will be an inspiration to other patients and will inspire you to keep up the good work also. When I had a graduate like you, I would invite that graduate to give my new group a pep talk on the first day of class. They need to hear someone like you because, as you may remember, they are not really sure they can be helped. Then, if you feel like it, attend other classes to keep motivating those new patients. You have more credibility than the staff does and this is a win-win job, helping everyone involved.
With best wishes for your continued success,
Mary Burns, RN, BS