
25 Feb When Should I Consider Oxygen Therapy for COPD?
by Christine Garvey FNP, MSN, MPA, MAACVPR
Starting supplemental oxygen therapy is both an important and complex decision. Given its complexity, understanding what this entails (including why and how it’s prescribed) and the pros and cons of using oxygen may be helpful. Your doctor, and often your lung specialist, should advise you why oxygen is recommended, and provide basics about what to expect, how to use it, and when to get a medical follow-up. This article describes some key areas related to using oxygen therapy for COPD and resources that may help you feel more prepared.
A low blood oxygen level (“hypoxemia”) is common in people with COPD, particularly those with more advanced disease, because of abnormalities in the lung’s ability to receive and transport oxygen into the blood flowing through the lungs. Hypoxemia may be present only during an activity such as walking, or both at rest and with activity. Low oxygen levels can be associated with shortness of breath, and if persistent and/or severe, impaired mental clarity, right heart strain (pulmonary hypertension), and, for some, worse survival. Supplemental oxygen is the most effective treatment for low oxygen levels. For those with low oxygen levels, along with quitting smoking, using supplemental oxygen is the most effective way to improve the quality and quantity of life. Additional patient resources on oxygen therapy and patient stories are available from the American Thoracic Society (ATS)
Over one million persons in the US have been prescribed long-term oxygen therapy (LTOT), which is defined as being prescribed oxygen for at least 15 hours per day. The decision to use oxygen begins with an assessment by your provider – usually a lung specialist. This should include oxygen saturation at rest and with activity. Oxygen saturation is the percent of the maximal ability of the red blood cells to carry oxygen in the arterial blood that is present at any given time. This is usually measured with a pulse oximeter, a small, clip-like device that attaches to a finger. Anyone considering using oxygen therapy should purchase an oximeter. The ATS also has an information sheet about pulse oximetry. You can also see an excellent video with PERF Board Member, Dr. Brian Tiep, explaining pulse oximetry here.
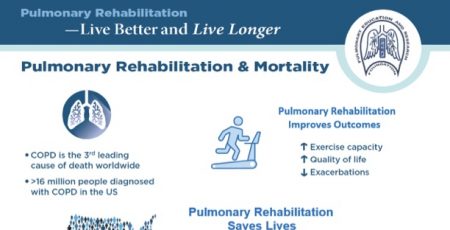
Most pulse oximeters intermittently monitor both oxygen saturation (SpO2) and heart rate. It is essential to learn how to properly monitor and interpret oxygen saturation. Most healthy people have oxygen saturation levels in the 95-98% range, although these levels may be lower for people living at altitude. Levels lower than 88-90% are often a reason for concern. Your lung specialist or primary provider needs to advise you on recommended SpO2 levels at rest and activity, as well as the amount of oxygen you are to use (in ‘liters per minute’) and when (e.g., during rest, exercise, and/or sleep), and if to use an oxygen device with continuous or intermittent oxygen flow. You should also be advised what to do if your oxygen saturation levels are below the recommended level. An important option for learning about the use of oxygen and an oximeter, as well as improving fitness, symptoms, and quality of life, is attending a pulmonary rehabilitation (PR) program. A program directory and information about PR are available at aacvpr.org and livebetter.org. Also, see our Basics pages for an overview of PR and exercising with COPD, as well information from other organizations on our Resources page.
If you are already using oxygen, you should be reevaluated by your provider using your own oxygen system. This should be done after prescribing oxygen, after any hospital admission, and at a minimum, every 6 months.
The primary reason that long-term oxygen is prescribed in most persons is its potential role in improving survival. Many who use oxygen breathe more comfortably. Understanding who will benefit most from LTOT was explored in a recent clinical practice guideline issued by the American Thoracic Society (ATS). Importantly, a guideline is not a prescription or mandate. It is a tool to help inform and guide clinicians. The final decision about using oxygen is shared between your provider and you, ideally once you are well informed about the pros and cons of oxygen therapy. The guideline recommendations included the following for persons with COPD:
- Recommend that LTOT be prescribed for those who have severe chronic resting hypoxemia defined as a SpO2 88% or lower (normally determined by pulse oximetry). [This recommendation was based on moderate-quality evidence.]
- Suggest LTOT not be prescribed for adults with COPD who have moderate chronic resting hypoxemia described as a SpO2 89–93%. [This recommendation was based on low-quality evidence.]
- Suggest ambulatory oxygen be prescribed for adults with COPD who have severe exertional hypoxemia such as while walking. [This recommendation was based on low-quality evidence.]
- Recommend that for all patients prescribed home oxygen therapy, both patients and their caregivers should receive training on the use and maintenance of all oxygen equipment and oxygen safety, including quitting smoking, fire prevention, and tripping hazards.
The ATS recommends the assessment of appropriate oxygen equipment based on your physical ability, health, lifestyle, and mobility needs. Safely using oxygen needs to be part of what your provider and oxygen supply staff, a durable medical equipment company (DME), provides. Below are examples of some safety recommendations.
- Quit smoking (ask your provider about help; also see our help pages). Never smoke or allow others to smoke or use e-cigarettes in the same room or within 6 feet of oxygen. Keep oxygen more than 6 feet away from open flames, such as matches, cigarette lighters, etc. Stay 6 feet away from heat sources, gas stoves, candles, fireplaces, electric or gas heaters, and anything that creates sparks.
- Don’t use flammable products like cleaning fluid, paint thinner or aerosol sprays near your oxygen supply.
- Keep oxygen containers upright. Larger ‘E’ cylinder tanks need to be stored in their carrying stroller or secured to prevent falling and danger from tank damage.
- When using oxygen, do no use products with oil, petroleum including Vaseline, grease, or other flammable products on your face, chest, hands, or upper body.
- Have a fire extinguisher close by that is not expired and be sure you are trained in its use.
- Post a sign on your door alerting others that oxygen is in use.
- If you use an oxygen concentrator, ask your utility company if you are eligible for priority service in case of a power failure or discounted utility rates.
An important aspect of oxygen therapy is the system for payment and providing home oxygen. Medicare overhauled its payment system in the past decade with a system called “Competitive Bidding”. Although the goals of the program included improved quality and cost containment, the latter is likely the primary outcome of this change. Liquid oxygen (LOX) historically provided small, lightweight portable containers capable of higher oxygen flow rates compared to tanks. Availability of portable LOX has declined dramatically in the past decade, reflecting lower Medicare payment to DMEs who now primarily provide oxygen tanks as portable or ambulatory oxygen. Heavier E cylinders in many cases are the primary portable system; these tanks must be pulled in a wheeled cart. The decline in the availability and adequacy of lightweight portable oxygen systems have impacted user mobility with reports of a decline in quality of life, mood, and increased isolation due to inadequate portable options (see the ATS Guideline for home oxygen therapy). These concerns have been brought to Medicare’s attention. It is unclear if this has resulted in improvement in any of the areas of payment, service, or equipment.
Oxygen devices normally produce and/or store oxygen. An oxygen concentrator separates oxygen from the nitrogen in the air (room air is approximately 21% oxygen and 79% nitrogen) to provide ‘concentrated’ oxygen to the user. Devices that store oxygen for use include oxygen tanks. Small tanks are lighter weight and may be easier for carrying and mobility, but contain less oxygen and therefore may not deliver oxygen for long periods and/or at high flow rates. Larger tanks, e.g., E cylinders last longer but are heavier (E-cylinders weigh up to 20 lb.) and require a stroller or rolling carrier for mobility and safety. Portable oxygen concentrators (POC) may provide lightweight oxygen delivery but most provide lower oxygen flow rates compared to tanks. Importantly, the POC setting or number that indicates oxygen flow has no relationship to the number of ‘liters per minute’ your doctor has prescribed for use of a continuous flow device. Most POCs deliver a maximum of 1 liter per minute or less excluding heavier devices such as SimplyGo, Eclipse, and a few other models. POCs may offer improved mobility, but users must regularly monitor SpO2 to be sure it is in the range prescribed by the provider. This is especially important during exercise or activity. POCs are the only oxygen system allowed on commercial flights. For more information, see our blog post on portable oxygen concentrators. Oxygen conserving devices may be used with tanks and are the only option with most POCs. This allows the oxygen supply to last longer, however, this type of oxygen delivery requires assessment by your provider or DME respiratory therapist to assure it provides you adequate oxygen levels, especially during activities such as walking.
Using oxygen has the potential to offer important benefits, along with some challenges. For example, did you know that it is possible to fly with supplemental oxygen? Discuss the pros and cons of oxygen therapy with your provider and be sure your questions are answered.




Jeff Padgett
Posted at 09:05h, 26 FebruaryThe article answered and made clear questions I had after the American Lung Associations Better Breathers Club meeting yesterday. The topic was about supplemental oxygen.
I do not currently use oxygen but I want to be well informed.
Thanks for the information and resources.
PERF
Posted at 11:34h, 26 FebruaryDear Jeff,
Thanks for your feedback! Our goal is to keep our readers informed and to help supplement the information you get from your support groups and physicians. We appreciate knowing we helped achieve that with you.
Mary Burns